11-14 Weeks (First Trimester) Perinatal Examination
EARLY ANOMALY SCREENING
9. Week
In these weeks of the first trimester, the embryo reaches 23-31 mm and embryo movements are observed. The body has turned into an elliptical structure with a large head. Abdominal wall is prominent, mouth can be seen, profile image can be taken. The extremities are elongated. Hands and feet are very close to each other and are in contact. The soles of the feet face each other in the sagittal plane. The lateral ventricles are prominent, while the choroid plexuses filling them can be best visualized in the parasagittal plane in 9 weeks and 4 days. They grow very rapidly simultaneously with the hemispheres and fill the entire ventricle. The cortex is smooth and hypoechoic. While the diencephalon cavity narrows, the mesencephalon is still wide. The lateral width of the rhombencephalon increases and it fills the cerebellum hemispheres, which are in two separate parts. In the ninth week, the heart rate increases and reaches 175 beats per minute. From the middle of the eighth week to the middle of the 10th week, all embryos show physiological intestinal herniation (Picture-6). This is best seen as a large hyperechoic mass at week 9. The diameter of the herniation is usually no more than 6.3 mm. By the end of the ninth week, the stomach can be seen in 75% of the embryos. Since the swallowing process has not started yet, the hypoechoic area seen is the physiological secretion of the stomach. Excessive dilation suggests esophageal and intestinal atresia.
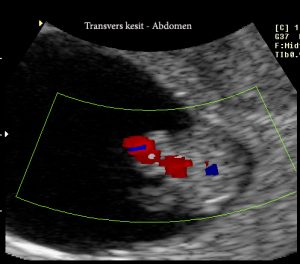
Fig-6
Content (Subtitles)



















10-11. Week
In these weeks at the beginning of the postembryonic period, the embryo reaches 34-42 mm (10 weeks) and 43-54 mm (11 weeks). The anterior head is protruding, the occiput is flat. The trunk is elongated. Hands and feet are distinguished. Feet are in their normal position. The lateral ventricles are in the shape of a crescent, filling the anterior part of the cranial cavity and hiding the diencephalic cavity (Pictures-7 and 8). While the diencephalon is located between the hemispheres, the mesencephalon displaces towards the middle of the cranial cavity (Picture-9). The third ventricle enlarges and then narrows. The cerebellar hemispheres are located in the midline. After 10 weeks and 3 days, the cerebellum and the choroid plexus in close proximity can be visualized in the 4th ventricle. In the eleventh week, ossification begins in the occiput, followed by the vertebrae (Picture-9). Moving valves, interventricular septum and vascular outlets are seen in the heart at the 10th week. The heart rate decreases to 165 per minute at the end of the 11th week. Physiological herniation regresses during these weeks and is not seen after 11 weeks and 5 days (Picture 10). The esophagus can be seen in two lines in front of the aorta. In all embryos, the stomach should be seen starting from the 11th week (Picture-11).
 Pic-7: Nuchal-Nape
Pic-7: Nuchal-Nape
 Pic-8: Fetal body image in midline section.
Pic-8: Fetal body image in midline section.
Pic-9: Early spine view (midline section).
 Pic-10: Omphalocele
Pic-10: Omphalocele
 Pic-11: Convex section and stomach observation.
Pic-11: Convex section and stomach observation.
FETAL ANOMALIES IN THE FIRST TRIMESTER OF PREGNANCY
Efforts to reveal the phenotypic features of Down syndrome by ultrasonography have been going on for years. Therefore, determination of fetal anatomy during fetal ultrasonography and early detection of anomalies, if any, have been put into practice as a clinical choice. During this examination; It is possible to detect an intrauterine pregnancy, to confirm the gestational age at an early stage, to diagnose early missed abortion, to reveal the chorionic structure in multiple pregnancies, to detect serious fetal anomalies, if any, and to perform chromosomal anomaly screening with nuchal thickness measurement.
10-14 days of pregnancy. Diagnosis of some severe fetal anomalies may be possible in weeks of gestation. Anencephaly, Encephalocele, Hydrocephalus, Holoprosencephaly, Meckel-Gruber Syndrome, Iniencephaly, Spina Bifida, Major heart anomalies, Omphalocele, Non-Gastroschia, Diaphragmatic Hernia, Renal agenesis, Infantile polycystic kidney, Hydronephrosis, Syndrome of the Hydronephroid system and Registry of the Skeletal system, Skeletal system anomalies Some other anomaly syndromes can be diagnosed.
A sensitivity of 50-60% has been reported in the diagnosis of structural anomalies by first trimester ultrasonography, and when second trimester screening is added to this method, the sensitivity is increased to 80%.
FETAL ANOMALIES IN THE FIRST TRIMESTER OF PREGNANCY
Efforts to reveal the phenotypic features of Down syndrome by ultrasonography have been going on for years. Therefore, determination of fetal anatomy during fetal ultrasonography and early detection of anomalies, if any, have been put into practice as a clinical choice. During this examination; It is possible to detect an intrauterine pregnancy, to confirm the gestational age at an early stage, to diagnose early missed abortion, to reveal the chorionic structure in multiple pregnancies, to detect serious fetal anomalies, if any, and to perform chromosomal anomaly screening with nuchal thickness measurement.
10-14 days of pregnancy. Diagnosis of some severe fetal anomalies may be possible in weeks of gestation. Anencephaly, Encephalocele, Hydrocephalus, Holoprosencephaly, Meckel-Gruber Syndrome, Iniencephaly, Spina Bifida, Major heart anomalies, Omphalocele, Non-Gastroschia, Diaphragmatic Hernia, Renal agenesis, Infantile polycystic kidney, Hydronephrosis, Syndrome of the Hydronephroid system and Registry of the Skeletal system, Skeletal system anomalies Some other anomaly syndromes can be diagnosed.
A sensitivity of 50-60% has been reported in the diagnosis of structural anomalies by first trimester ultrasonography, and when second trimester screening is added to this method, the sensitivity is increased to 80%.
HEART ANOMALIES
It is the most common congenital anomaly and its frequency at birth is approximately ‰ 3-4. Half of these are lethal or major anomalies requiring surgery. A 4-chamber view of the heart can be used as a screening test in ultrasonographic examination. However, only 25-60% of major cardiac anomalies can be recognized with this method. At the 13th week of pregnancy, this image could be revealed in 100% of cases transvaginally. Bronshtein et al. At 13 weeks, Fallot reported a diagnosis of tetralogy. Achiron et al. reported 8 cases with major cardiac anomalies (ectopia cordis, wide right atrium, atrioventricular septal defect) at 10-12 weeks. In the screening of congenital heart diseases, 1st trimester ultrasonography gives limited results just like 2nd trimester sonography.
In a study performed in 112 cases with chromosomal anomaly (60 cases trisomy-21, 29 cases trisomy-18, 17 cases trisomy-13 and 6 cases XO) detected by nuchal test at 10-14 weeks of pregnancy, the presence of nuchal thickness and cardiac anomalies were examined. In another study, cases with increased nuchal thickness but with normal chromosomes were examined. In these cases, the diagnosis of cardiac anomaly was made by second trimester ultrasonography, autopsy examination or the necessary examination methods at birth. Considering its relationship with nuchal thickness; Major cardiac anomaly is ‰5 in patients with a nuchal thickness less than 3.5 mm, while it is ‰23.3 in those with a nuchal thickness of 5.5 mm or more. These findings suggest that the nuchal thickness test may be a good screening test for major cardiac anomalies. Therefore, cases with increased nuchal thickness but with normal chromosomes, 20-24. should be sent to the relevant Perinatology Specialist for fetal echography at the gestational week.
CENTRAL NERVOUS SYSTEM ANOMALIES
Exencephaly, which is a result of peering, results in anencephaly with advancing gestational weeks. The absence of the calvarium and cerebral hemispheres is the basis for the diagnosis of anencephaly in the 2nd or 3rd trimester of pregnancy. The calvarium ossifies after the 10th gestational week and is observed as hyperechoic after the 11th week by ultrasonography (Picture-12). In the absence of the calvarium, this hyperechoic area cannot be seen, but the hemispheres are seen normally. This situation shows acrani (exencephaly) (Picture-13). Due to the irregular contour, this situation can be suspected for the first time at the 8th gestational week. If these findings are taken into consideration, the 12-14th day of pregnancy. Anencephaly can be easily diagnosed in
Picture-12: Observation of the cranium.
Picture-13: Akrania view.
At the 11th week of pregnancy, the diagnosis of encephalocele can be made with irregularly circumscribed head structure, cystic formations and microcephaly together. Encephalocele is also a manifestation of Meckel-Gruber syndrome, and tissues protruding from the posterior fossa via the occiput can be shown in the last days of the embryonic period. This condition was suspected by detecting an enlarged rhombencephalon at 8 weeks and 5 days at the earliest.
Although its early diagnosis is difficult (25%), shaking of the choroid plexuses suggests hydrocephalus. There are single ventricle (alobar), partial segmentation or lobar types. The thalamus may be fused or separate. Facial anomalies may accompany (single orbit, cleft palate…). Trisomy 13 is the diagnosis to be considered. There is increased nuchal thickness in 76% of fetuses with trisomy 13, and tachycardia is present in 24%. Hydrencephaly was also recognized at 12 weeks of gestation. There is an enlarged head, small hemispheres, and the appearance of a fluid-filled cranial cavity with no midline echo.
In Dandy-Walker malformation with complete or partial defect of the fourth ventricle and cerebellar vermis, it is estimated that the event begins in the membranous area where the cerebellar hemispheres meet. This type of defect was shown at the earliest 11th gestational week. It is associated with chromosomal abnormalities or fetal infection.
Usually (75%) encephalocele (brain) or meningocele (meninges) arising from the occipital region can be recognized after the 10th week when cranial ossification begins. In addition to the sac structure, bone defect can also be shown.
As it is known, the neural canal closes normally at the 6th week of pregnancy and as of the 10th week of pregnancy, the vertebrae are observed normally by ultrasonography, and a triple ossification image is obtained. It can be observed that the vertebrae are covered with skin in both the transverse and coronal planes. In the presence of spina bifida; vertebrae cannot be observed covered by skin, triple ossification image cannot be detected, “V” shaped opening is detected, straight vertebral image cannot be observed (Picture-14). Scoliotic and kyphotic images are detected at the level of the opening (Picture-15). In addition, “Banana” and later “Lemon” images can be detected in some of the spina bifida cases at 12-14 weeks of gestation. Disruption of parallelism in the tissues that will form the smaller rhombencephalic space and spina can be suspected as the first finding, especially in large meningomyelocele cases.
 Figure-14: Spina bifida image in transverse section.
Figure-14: Spina bifida image in transverse section.
 Figure-15: Image of spina bifida in sagittal section.
Figure-15: Image of spina bifida in sagittal section.
FACIAL ANOMALIES
At the end of the embryonic period, the eyes, maxilla and mandible can be distinguished. Proboscis, cyclopia and advanced hypotelorism, which can be seen with holoprosencephaly, can be easily detected in these weeks.
DIAPHRAGMA HERNIA
The development of the diaphragm is completed in the 9th week. When there is a developmental defect, the intestines return from the umbilical cord into the abdomen. Abdominal organs herniate into the thoracic cavity from the defect site. About half of diaphragmatic hernias are accompanied by chromosomal anomaly or other anomalies. In the neonatal period, 50% of the cases die due to lung hypoplasia and pulmonary hypertension. In the series of 78639 cases of Sebire et al., nuchal thickness was found to be pathological in 37% of diaphragmatic hernia cases. The increased nuchal thickness is explained by the severe venous return difficulty caused by herniation of the abdominal organs in the thorax. When these cases were evaluated within themselves, it was determined that nuchal thickness increased in 83% of neonatal losses and in 22% of survivors. However, it is known that the prognosis of diaphragmatic hernias occurring in late pregnancy periods is good. Diaphragmatic hernia should be kept in mind in the increased nuchal test detected by early pregnancy ultrasonography.
GASTROINTESTINAL SYSTEM AND ABDOMINAL WALL DEFECTS
Obstructions
While obstructions may cause dilatation in the intestines, tumors or cysts are not seen much in the first trimester of pregnancy. Blaas and Eik-Nes detected a dilated stomach (6 mm) at 10 weeks and 5 days in a fetus in a triplet pregnancy, and observed that the stomach was always empty after the 12th week. A diagnosis of fistula-free esophageal atresia was made after birth. Tsukerman et al. 12-13 of pregnancy. described a case in which esophageal atresia and duodenal stenosis were found together. They suggested that in this period, when swallowing has not started yet, the existing dilated structures are filled with gastric secretion.
Omphalocele
As mentioned earlier, all embryos are born between 8-10 days of pregnancy. They show physiological bowel herniation at weeks 10-12. The 11th week ends in 5 days, with the return of the hyperechoic abdominal organs to their normal anatomical localizations. If this herniation still continues in the 12th week, it is called omphalocele (Picture-16). In the presence of omphalocele, additional anomalies and chromosomal anomalies (especially trisomy 18) should be investigated. If the week of diagnosis is 12, the probability of chromosomal anomaly is 50%, if the week of gestation is 20, 30%, and 15% at birth. Its incidence, again, varies according to the gestational week. The frequency is 1/1000 at the 12th week of pregnancy, 1/3000 at the 20th week and 1/3500 at the birth. Therefore, early diagnosis of omphalocele gains importance in this respect. Increased nuchal thickness was found in 57% of omphalocele cases detected in the first trimester, and chromosomal anomaly was not observed in any case with liver. Pentalogy of Cantrell, which includes epigastric omphalocele, diaphragm, pericardium, sternum and heart defects together, was defined in the first trimester. Such conditions can be recognized from the 9th week of pregnancy.
 Picture-16: Omphalocele image.
Picture-16: Omphalocele image.
Gastroschisis
It is an anomaly characterized by the fact that the intestines protrude freely into the amnion through a small wall defect just right of the umbilicus (paraumbilical), affecting all layers of the abdomen, and the umbilical cord is detected in its normal place in an average of 1 case in every 5000 births. In addition, some gastrointestinal anomalies may be found. The probability of chromosomal anomaly is very low.
Complex Wall Defects
(Limb-body-wall complex, Amnion rupture sequence)
It is a wide spectrum characterized by short cord and wall defects, joint defects of the extremity, vertebrae, face, and cranium, characterized by adherence to the amnion and persistence of extraembryonic coeloma. The abnormal amniotic cavity can be recognized at 8-12 weeks by the appearance of the heart outside the thorax and the lower part of the body in the coelom. In 71% of these fetuses, nuchal thickness increased, but chromosome analysis was found to be normal.
Bladder Exstrophy
Although the diagnosis is not reported in the first trimester, the absence of the bladder after the 12th week may raise suspicion.
URINARY SYSTEM ANOMALIES
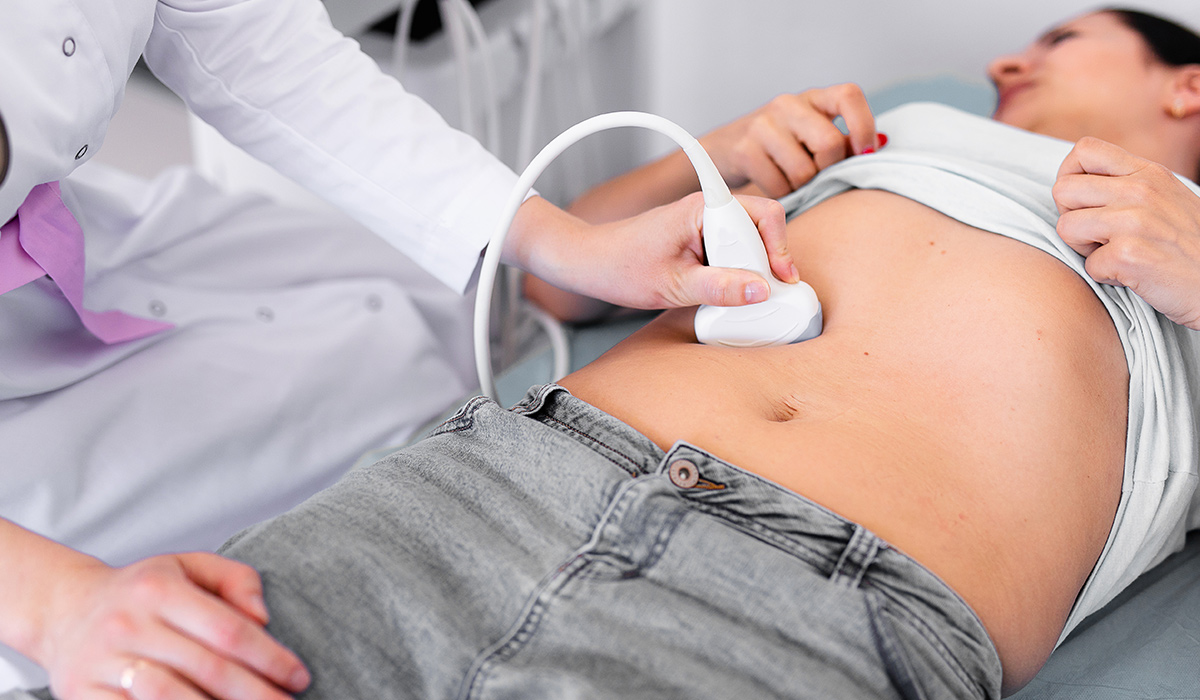
Despite the presence of urinary system defects in the early stages of pregnancy, oligohydramnios is not seen. The fluid coming from the amniotic membrane by diffusion makes the amniotic fluid. Fetal urine joins this system only after the 10th week. With transvaginal ultrasonography, it is possible to visualize the fetal bladder in 80% of the cases at the 11th week and in 92% of the cases at the 13th week (Picture-17). Braithwaite is 12-13 with transabdominal or transvaginal ultrasonography. reported that it is possible to visualize fetal kidneys in 99% of the cases (Pictures-18 and 19). Likewise: hydronephrosis, pyelectasis and renal agenesis can also be recognized during these weeks. From this point of view, it is possible to diagnose serious anomalies of the urinary system that occur in the early period. With careful examination, the diagnosis of infantile polycystic kidney and multicystic kidney can be made (Picture-20). Observation of bilateral hyperechogenic kidneys and accompanying oligohydramnios makes the diagnosis of infantile polycystic kidney. In multicystic dysplastic kidney, on the other hand, a hyperechoic image with cystic structure of different sizes bilaterally or unilaterally dominates the picture. When bilateral, the bladder cannot be observed and may be accompanied by oligohydramnios. It should be known that diagnosis is possible at 10-14 weeks of pregnancy. However, a negative finding does not mean that these anomalies will not be seen in the future.
Figure-17: Early mid-sagittal view and bladder.
Picture-18: Fetal bladder view.
Figure-19: The view of the kidneys in transverse section.
Picture-20: Infantile polycystic kidney.
Polydactyly, bilateral polycystic kidney and encephalocele observed in autosomal recessive Meckel-Gruber Syndrome can be easily detected at 10-14 GW. It is possible to observe all three parameters with transabdominal ultrasonography at 12-14 weeks of pregnancy. Megacystis also gains importance at 10-14 weeks of pregnancy (Picture-21 and 22). In their series of 300 cases, Sebire et al. observed the fetal bladder in all cases with a CRL measurement of 67 mm and above, and they determined a maximum measurement of 6 mm. In addition, 50% of the 16 megacystises detected by the same study group disappeared spontaneously, obstructive uropathy developed in 30% in the future, and chromosomal anomaly was detected in 20%.
Picture-21: Megacystis.
Picture-22: Megacystis and shunt application.
Skeletal System Anomalies
Extremity outlines at 8 weeks, 9-10, with early ultrasonography. Long bones can be seen in weeks, and fingers can be seen from 11 weeks. Lethal skeletal system anomalies can be diagnosed more easily in the 2nd trimester, however, there are also skeletal system anomalies diagnosed in the 1st trimester. It has been reported that it is possible to diagnose anomalies such as Type 2 Achondrogenesis, Tanatophoric dwarfism, Osteogenesis Imperfecta, Jeune’s syndrome, Roberts and Jarcho-Levin syndrome, FADS (Fetal Akinesia Deformation Sequence), Arthrogryposis in early pregnancy. Incompatibility between trunk and extremities, short extremities, immobility in extremities, fractures, mineralization defect in cranium, vertebrae and extremities, misalignment of vertebrae and ribs, clubfoot, increased nuchal thickness and edema are guidelines for early diagnosis. However, it should not be forgotten that some defects will show symptoms in the late periods.
Various researchers have reported that anomalies such as Smith-Lemli-Opitz, Caudal Regression, Hydrocephalus and Amniotic Band Syndrome can be diagnosed at 10-14 weeks of gestation.
MALFORMATIONS AND EARLY ULTRASONOGRAPHY
Whitlow et al., in a study they conducted in recent years, emphasized that structural anomalies in the fetus can be detected by ultrasonography at a rate of 59% in the early period (11-14 weeks). They found 1.4% structural or chromosomal anomalies in their group (n: 6634) that they examined on the mean of 12 weeks and 4 days of pregnancy. Chromosomal anomalies accounted for 46% of the anomalies they detected, and structural anomalies for 54%.
CHROMOSOME ANOMALIES AND EARLY ULTRASONOGRAPHY
Sonography findings that may raise suspicion for chromosomal abnormalities in early pregnancy have attracted the attention of many researchers and various studies have been published. In this section we will examine those that may be associated with them.
It was investigated whether short CRL, which we can call restricted development or developmental delay in early periods, could be a precursor for chromosomal anomalies, between the 64th and 86th days of pregnancy according to SAT, and CRL values were compared in 500 control cases and 25 chromosomal anomaly cases. It has been stated that CRL measurement cannot be a screening test for chromosomal anomalies other than tripliody, and developmental restriction in trisomy 18 and trisomy 21 can only be detected after the 12th gestational week. In a smaller number of series, the CRL measurement found with the expected CRL measurement was compared in abortions with and without chromosomal normality, and it was emphasized that CRL measurement did not have a distinctive value for chromosomal abnormality. As a matter of fact, morphology studies carried out in early abortions also yielded findings in this direction. However, in a larger study conducted by Schemmer et al. in recent years, 196 chromosomal anomalies were examined and it was emphasized that the mean CRL measurement was lower than normal, especially in trisomy 13, 18 and triploidies. The authors argued that assessment of growth rate is a better indicator than a single measurement of CRL.
In Italy, 1331 cases with risk for malformation and genetics were examined by transvaginal ultrasonography in the early stages of pregnancy, and it was concluded that the structural anomalies found could not be effective markers for early recognition of chromosomal anomalies. In the study of Rosati et al., in which they examined the relationship between cerebellar diameter or cisterna magna measurements and chromosomal abnormality, it was suggested that early ultrasonography did not yield significant results in terms of screening.
In studies conducted in the 1990s, screening examination of fetal heart rate was not found useful in the early diagnosis of chromosomal abnormalities. However, in the study of Jauniaux et al., it was stated that the heart rate was higher in fetuses with trisomy 21 compared to the others.
MULTIPLE PREGNANCY
It is known that; While the rate of missed abortion in singleton pregnancies is 1.8%, it is .2.8% in twins and 5.4% in triplets. In missed abortion cases, both fetuses are found to be dead in all monochorionic and 20% bichorionic twins. A fetus was found dead in 17% of bichorionic twins who also aborted. Based on the weeks of pregnancy; While the abortion rate is 12.2% in monochorionics at 12-24 GH, it is 1.8% in bichorionics. Perinatal mortality is 2.8% in monochorionic and 1.6% in dichorionic. The incidence of growth retardation is 21% in monochorionics and 5.5% in dichorionics. As can be seen here, there is a marked difference in prognosis between monochorionics and bichorionics. The easiest and most accurate determination of chorionicity is at 10-14.GH. In monochorionics, ultrasonographic identification is given as a “T” sign at the junction of the common membrane with the placenta (Picture-23). However, in dichorionics, lambda is defined as the “Λ” sign (Picture-24). Where there is a common membrane, the chorionic tissue of both placentas appears as Λ between both membranes, and as the gestational week progresses, it disappears with pressure after the 14th week and turns into a “T” shape as in monochorionic ones. For this reason, the “Λ” sign will be detected in dichorionics at 10-14 GH. This finding constitutes a valuable ultrasonographic parameter in terms of chorionicity. Chorionicity is important in terms of pregnancy prognosis and twin-to-twin transfusion and genetic counseling. In a singleton pregnancy where the risk of Down Syndrome is 1/200, the risk of trisomy-21 for monozygotics is 1/200 for one or both fetuses in the same sample, while it is 1/100 for a single fetus and 1/40,000 for both fetuses in dizygotic cases. As a result of the probability obtained by nuchal thickness measurement, a separate risk of trisomy-21 can be calculated for each fetus. This is decisive for the indication of invasive test.
Picture-23: T-symptom-Monochorionic twin pregnancy.
Picture-24: Lambda sign – Dichorionic pregnancy.
NUKAL TEST AND CHROMOSOME ANOMALIES
Various screening methods have been developed for Down syndrome, the first of which was advanced maternal age. At first, pregnant women over the age of 37 and later on formed the risk group for Down syndrome. It was aimed to diagnose Down syndrome by performing amniocentesis in this group of pregnant women. However, this group of pregnant women constitute only 5% of the general population and 30% of the babies born with Down syndrome. The rest are born from pregnancies under the age of 35. In order to diagnose babies with Down syndrome in this group in early pregnancy periods, 16-21. AFP, UE3, HCG biochemical parameters measured between gestational weeks have been put into practice. This test is aimed to determine the pregnancies that constitute a risk group for Down syndrome by evaluating the triple parameter with maternal age. With the Triple Screening Test, only 60% of pregnancies with Down syndrome can be recognized. For this reason, other scanning methods have been the subject of research. Among the first trimester biochemical parameters, beta-HCG and PAPP-A have now taken their place in clinical practice. 11-14 on the other hand. The measurement of nuchal thickness in the ultrasonographic examination performed during the gestational weeks has taken its place as an effective screening test not only in Down syndrome, but also in other chromosomal anomalies and even non-chromosomal fetal anomalies. 11-14 days of pregnancy with maternal age. The nuchal screening test, which is 80% effective against 5% invasive test in chromosomal anomalies with the evaluation of the nuchal thickness measurement in the first weeks of gestation, was defined by Nicolaides. When beta-hCG and PAPP-A are added to the nuchal thickness, the efficiency rises above 90%.
Nuchal thickness measurement, 11-14. It can be easily done with transabdominal ultrasonography during pregnancy weeks. However, sometimes adequate images cannot be obtained in obese patients and transvaginal ultrasonography can be applied under these conditions. 11-14 days of pregnancy. The position and posture of the fetus in weeks of gestation are quite suitable for the measurement of apical-breech (CRL) and nuchal thickness by transabdominal ultrasonography (Picture-25, 26 CRL measurement). In nuchal measurement, when the following points are taken into consideration, both the most accurate and the easiest and fastest measurement will be made. The fetus must be visualized to cover at least ¾ of the screen. As the plan, the sagittal plane should be taken, in which the spinae can be seen along the entire line. This plan is also the plan required for CRL measurement. This feature should be easily known and applied by all sonography practitioners. The other issue is; is to distinguish between fetal skin and amniotic membrane, that is, to observe them separately. Failure to do so will result in erroneous measurements. If spontaneous fetal movements are expected, or if the fetus is moved by coughing the pregnant woman or by gently blowing the abdominal wall with the fingertips on the uterus, separation of the fetal skin and amniotic membrane can be observed and displayed separately.
In general, at this gestational week, the fetus lies in a hammock on the amniotic membrane. Both CRL and nuchal thickness are measured in the sagittal plane and under conditions where the fetal skin and amniotic membrane are imaged separately. The distance to be measured is between the fetal skin and the soft tissue covering the spinae. During these gestational weeks, both structures appear as a thin membrane. Membranes will become better visible by not creating too much echogenicity. In these conditions, the measurement is obtained by marking on both membranes. The maximum measurement thus obtained is based on. At the same time, the nuchal thickness, CRL, and the image on the amniotic membrane should be printed and stored in the patient’s file. The resolution level of ultrasonography devices produced in recent years is sufficient to obtain clear and accurate images. It has been a matter of debate whether there is a difference between practitioners who measure. It was found that there was a difference of 0.54 mm between the two measurements and 0.62 mm between individuals. Accurate measurement is unavoidable if attention is paid to careful placement of the marking on the membranes, based on the case where the membranes are visible separately, observing the sagittal plan, and covering at least ¾ of the screen of the screen. During the inspection, it would be appropriate to verify with several consecutive measurements. The nuchal thickness measurement with these conditions can be easily done by any practitioner who can measure CRL.
Picture-25-26: CRL measurement.
The nuchal thickness shows increasing parallelism with the gestational week. For this reason, the nuchal thickness normal will change according to each gestational week. However, if you want to give a rough figure, 2.5 mm average is the normal acceptable limit. However, even so, it is not correct to evaluate the nuchal measurement as normal or pathological and should not mean anything by itself. Because the current risk increases with the increase of nuchal thickness or decreases with its decrease. The more the nuchal thickness deviates from normal, the greater the risk. The greater the deviation from the normal nuchal thickness, which is specific to each gestational week, the more it corresponds to a varying probability coefficient. The new risk is calculated by multiplying this coefficient with the current risk. A computer program has been developed for these calculations. Ultrasound users, who successfully completed the early fetal ultrasonography courses jointly established by the Fetal Medicine Foundation from England, Turkish Perinatology Society and the Obstetrics and Gynecology Ultrasonography Association, and then completed their practical training in the relevant centers, receive certificates for their training on the relevant subject and computer programs for use in clinical applications. providing assistance. At regular intervals, the work of these users is supported and supervised by both organizations. Thus, difficulties in practice are helped and the latest knowledge is added.
The King’s College group, which published their studies, found nuchal thickness above the 95% percentile in 80% of trisomy-21 cases in a series of 1273 cases. Similar results were obtained in subsequent studies. In a multicenter study of 20804 cases performed at 10-14 GH as a screening program; It has been reported that nuchal thickness increases with gestational age in normal pregnant women, and increased nuchal thickness is detected in chromosomal anomalies. Again, it was determined that the calculated risk in 5% of the cases was 1/100 or more and 80% of these cases were trisomy 21 and 77% had other chromosomal anomalies. As of June 1997, the number of pregnant women screened by a multi-center study composed of 27 centers from different countries, organized by the Fetal Medicine Foundation, reached 100,311. In this study, the efficacy for trisomy 21 was around 82% when a threshold value of 1/300 was taken. For other chromosomal anomalies, it varies between 65% and 89%.
The parameters used in the nuchal test are maternal age, gestational age, history of baby with trisomy, nuchal thickness and ultrasonographic fetal anomaly findings. As it is known, in cases with a baby with trisomy anamnesis, the current risk (existing risk according to maternal age and gestational week) is added to 0.75% to calculate the new risk. A new risk is found by multiplying the coefficient obtained by the nuchal thickness measurement with the last risk. If there is a separate coefficient for each of the fetal anomalies detected in the ultrasonographic examination, and the final risk value is found by multiplying with the last risk at hand. This method is called “Sequential Scan”. When beta-hCG and PAPP-A are added to the nuchal screening program at 11-14 weeks, the effectiveness for trisomy 21 rises above 90%.
In addition, Doppler, nasal bone, facial angle, cardiac examination and early anatomy examination, as well as more sensitive and highly specific perinatal ultrasound examination, which is applied in Perinatology Centers, have now been put into practice. In cases where the Down Syndrome risk calculated by nuchal thickness and biochemistry is less than 1/1000, the majority of pregnant women agree that the risk is at an acceptably low rate. However, in cases with a risk greater than 1/1000, there are difficulties in deciding on the invasive test. In these cases, the 11-14 week examination by the Perinatology Specialist largely resolves this situation. As a matter of fact, an advanced Perinatal Ultrasound examination contributes to the solution by revealing nuchal thickness, nasal bone, ductus venous, tricuspid regurgitation, facial angle, minor or major ultrasound markers and anomalies.
INCREASED NUCAL THICKNESS AND NON-CHROMOSOMAL ANOMALIES
In a study conducted in the periods before the current understanding of nuchal thickness was established, cystic hygromas with and without septation were compared and the following results were obtained. Cystic hygroma was detected in 125 of 7582 fetuses without septation, and cystic hygroma with septation in 25 of them, 98% of those without septation and 44% of those with septation disappeared in the future. Both structural and chromosomal anomalies were found more in the group with septation.
In a series of 565 cases with increased nuchal thickness and normal chromosomes; Cardiac anomalies, diaphragmatic hernia, kidney and anterior abdominal wall anomalies were found at a rate of approximately 4% and were higher than the normal population. On the other hand, in cases with increased nuchal thickness and observed as nuchal edema in later weeks of gestation; It has been reported that the risk of rare genetic syndromes such as Stickler syndrome, Smith-Lemli-Opitz syndrome, Jarco Lavine syndrome, and arthrogryposis is high. Necessary information about anomalies detected at 11-14 weeks of early pregnancy were discussed in the sections above. Considering the relationship between increased nuchal thickness, perinatal deaths, and survival determined based on evacuations due to fetal anomalies; While survival is 97% in cases with 3 mm nuchal thickness, it is reported as 53% in cases with nuchal thickness greater than 5 mm. As a result, nuchal test at 11-14 GW with maternal age replaces the most effective screening test for trisomy-21 with a sensitivity of 82%. It is a viable screening test for multiple pregnancies. It is also reported to be a good screening test for other chromosomal anomalies (Trisomy 18, 13, Turner, Triploidy and sex chromosome anomalies…) with a sensitivity ranging from 65% to 82%. Likewise, its usefulness in early detection of genetic syndromes is obvious.
With the provision of sufficient knowledge and education on early pregnancy ultrasonography, the way for routine clinical applications is cleared. With good practice, both the sensitivity of ultrasonography will increase and the number of unnecessary invasive procedures can be reduced.
Prof.Dr. Cihat Şen